Root canals have historically gotten a bad rap, but they can be the saving grace for your extreme tooth pain, and the tooth itself! When many people think of root canal therapy, they fear the dentist or endodontist causing intense pain. However, that is not the case! In fact, root canals help to eliminate your tooth pain and are not a painful procedure.
Why do I need a root canal?
A root canal is typically necessary when the dental pulp inside a tooth becomes infected or damaged. The dental pulp is the soft, innermost layer of the tooth that contains nerves, blood vessels, and connective tissue. Several factors can lead to the need for a root canal:
- Tooth decay: If tooth decay is left untreated, it can progress deep into the tooth, reaching the dental pulp. Bacteria from the decay can infect the pulp, leading to inflammation, pain, and infection.
- Dental trauma: A tooth that has suffered significant physical trauma, such as a fracture or a strong impact, can damage the dental pulp. Even if there are no visible cracks or chips, the trauma can cause the pulp to become inflamed or infected over time.
- Dental infections: In some cases, untreated cavities or dental infections can spread to the dental pulp, causing an infection. This can occur when the infection reaches the root canals through the tiny tubules in the tooth’s dentin.
- Repeated dental procedures: If a tooth has undergone multiple dental procedures, such as fillings or crowns, it can weaken over time and make the dental pulp susceptible to infection.
- Cracked or fractured tooth: A cracked or fractured tooth can expose the dental pulp to bacteria, leading to infection and inflammation.
The purpose of a root canal is to remove the infected or damaged pulp, clean the root canals, and seal them to prevent further infection. By preserving the natural tooth structure through a root canal, it’s possible to save the tooth rather than extracting it. Saving the tooth is beneficial for maintaining proper chewing function, preventing surrounding teeth from shifting, and avoiding the need for tooth replacement options like dental implants or bridges.
Root canals are needed to remove bacteria and infected tissue from a tooth’s infected root. Performing root canal therapy prevents reinfection and can help save the natural tooth. If you are experiencing any of the following symptoms, a root canal may be the answer:
- Severe pain while chewing or biting
- General trauma to the tooth, such as a chipped or cracked tooth
- Lingering sensitivity to hot or cold, even after the sensation has been removed
- Aching or constant throbbing pain in the mouth
- Swollen or tender gums
- Deep decay or darkening of the gums
What happens during a root canal?
Today’s root canals are very similar to a routine dental filling and are not painful. Often the pain from your tooth is worse than the actual procedure. The procedure, given proper anesthesia, has no pain at all! After treatment, you will be pain-free and on your way to recovery.
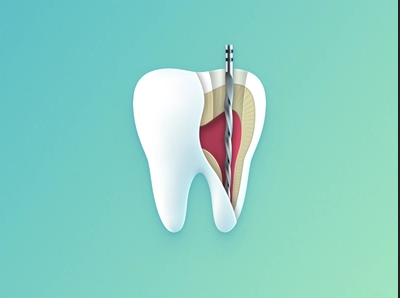
During a root canal procedure, a dentist or an endodontist (a specialist in treating dental pulp) removes the infected or damaged pulp from the interior of a tooth. Here’s a step-by-step explanation of what typically happens during a root canal:
- Preparation: The dentist will administer local anesthesia to numb the area around the affected tooth, ensuring you don’t experience pain during the procedure. A dental dam, a thin sheet of rubber, may be placed around the tooth to isolate it and keep it clean.
- Accessing the pulp: The dentist creates a small opening in the tooth’s crown, usually using a dental drill. This access point allows them to reach the pulp chamber and root canals.
- Removing the infected pulp: Using specialized dental instruments called files, the dentist carefully removes the infected or inflamed pulp tissue from the pulp chamber and root canals. They may also use an antimicrobial solution to disinfect the area and ensure any bacteria are eliminated.
- Shaping and cleaning the canals: The dentist uses tiny files of increasing sizes to shape the root canals, removing any remaining infected material and preparing them for filling. This step is important to prevent future reinfection.
- Filling the canals: Once the canals are cleaned and shaped, they are filled with a biocompatible material called gutta-percha. Gutta-percha is a rubber-like material that seals the canals to prevent further infection.
- Restoring the tooth: After the root canal is completed, the access opening in the tooth is sealed with a temporary or permanent filling. In some cases, a dental crown may be recommended to provide additional strength and protection to the tooth, especially if it’s extensively decayed or weakened.
- Follow-up: You will typically be scheduled for a follow-up visit to the dentist. During this appointment, the dentist will check the tooth’s healing progress and may place a permanent crown if necessary.
It’s important to note that while root canals have a reputation for being painful, modern techniques and anesthesia ensure that the procedure is generally comfortable and relatively painless. After the root canal, you may experience some mild soreness or discomfort, which can be managed with over-the-counter pain medications.
Your dentist or endodontist will begin by numbing the area. They then remove the inflamed or infected nerve of the tooth. The area is then filled and sealed to prevent repeat infection. Afterward, you will likely need a crown placed on the treated tooth to restore full form and function.
Run don’t walk!
Don’t let your fear of the dentist or root canals keep you from becoming pain-free. The longer you wait, the more pain you will experience and can sometimes result in losing the tooth if not treated. This also risks greater and worsening infection.